Best doctor for fissure in Hyderabad
Dr. Datta Ram explains everything about anal fissure that you always want to know.
ANAL FISSURES – Causes, Symptoms & Treatment
Anal Fissure: A small tear in the thin, moist tissue that lines the anus is known as anal fissure. It causes pain and bleeding with bowel movements. Anal fissures can occur in people of any age. In many cases, they get better with some home-based remedies such as warm-water bath sitz; increasing fiber intake; taking medications. Surgery may be recommended in some cases.
What are the causes of anal fissures?
Anal fissure causes include:
- Constipation
- Passing large and hard stools
- Straining during bowel movements
- Childbirth (women)
- Long-lasting diarrhea
- Anal intercourse
What are the symptoms of anal fissure?
Anal Fissure symptoms may include:
- A crack or tear in the skin around the anus
- A skin tag or small lump in the skin near the fissure
- Bright red blood on stool or on toilet paper after a bowel movement
- Pain during and after bowel movements
What are the risk factors for anal fissure?
The factors that may increase the risk of anal fissure include:
Age: Common in infants and middle-aged adults.
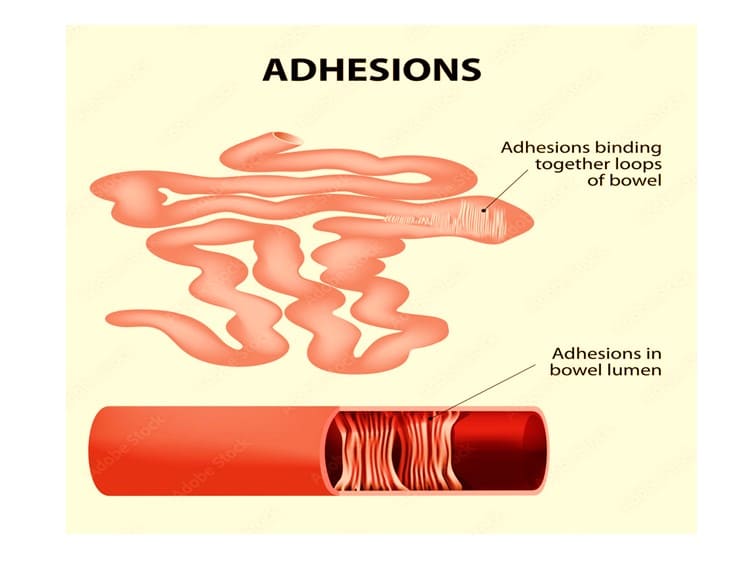
Crohn’s disease: It can make the lining of anal canal susceptible to tearing.
Childbirth: The risk of anal fissure increases after childbirth in women.
Constipation: Passing hard and bulky stools and straining during bowel movements can increase the risk of tearing anal skin.
Anal intercourse increases the risk of anal fissures.
What happens if you don’t treat anal fissures?
Chronic anal fissure fails to heal up to several weeks – may be up to six to eight weeks. It needs comprehensive treatment.
Untreated fissure and fissure that extends into the ring of muscles that keeps anus closed may become problematic. Once a fissure enters into the internal anal sphincter, it becomes difficult for it to heal. When this happens, you may need medicines to ease the discomfort. And to reduce the pain or remove the fissure, you will need surgery.
Treatment
The treatment for anal fissure depends on the severity of the condition and associated symptoms. The non-surgical approaches may include external application of nitroglycerin if other conservative approaches fail to give any relief. In addition, doctors may also prescribe topical anesthetic creams to relieve pain.
Surgery: If conservative treatment approaches fail to give any results, your surgical gastroenterologist may recommend surgery. The doctor will perform lateral internal sphincterotomy (LIS). If the symptoms are severe, then this procedure may help relieve pain, reduce spasm and promote healing.