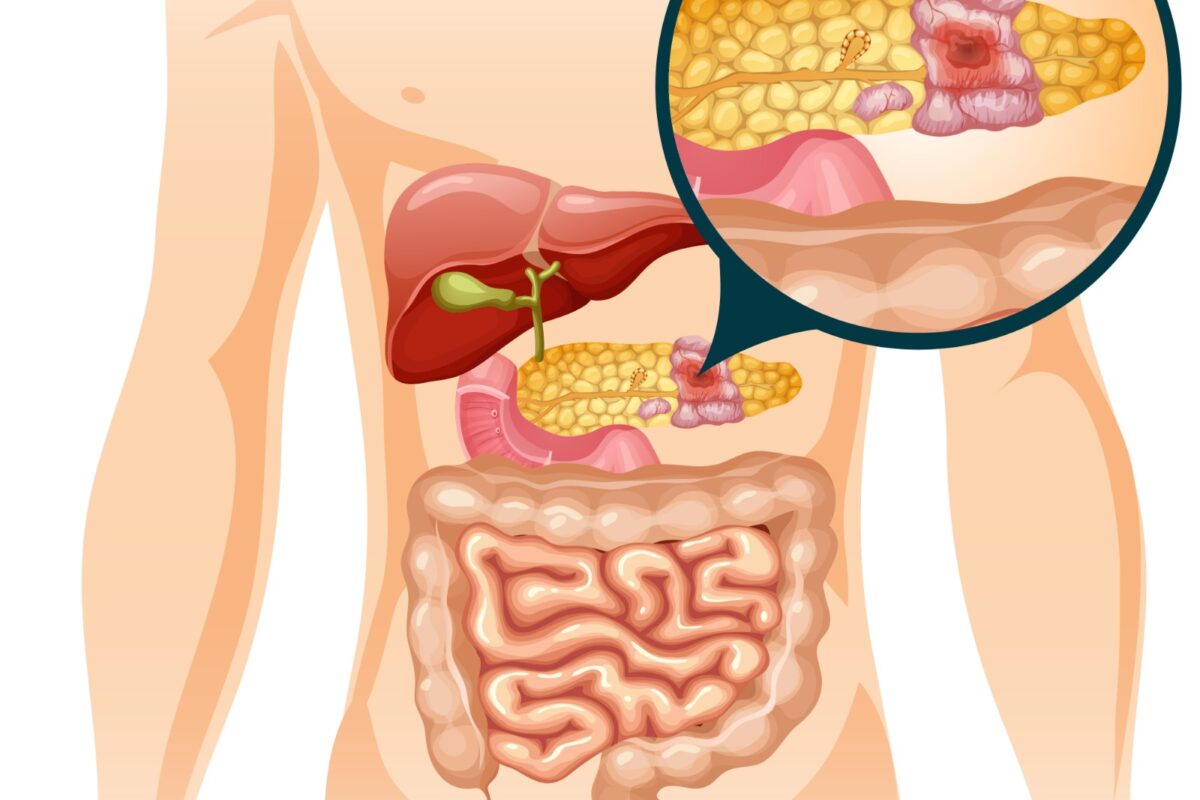
Pancreatic cancer is a type of cancer that starts as an abnormal growth of cells in the pancreas. The pancreas is situated behind the lower part of the stomach. Enzymes and hormones that help digest food and help control blood sugar are made in the pancreas.
The most common type of pancreatic cancer is pancreatic ductal adenocarcinoma.
It is rarely found at an early stage when the chances of getting cured are higher. This is because the symptoms take time to manifest until then the cancer has spread to different organs.
Pancreatic cancer treatment in Hyderabad: The options for pancreatic cancer include – surgery, chemotherapy, and radiation therapy.
Symptoms
Pancreatic cancer doesn’t cause any symptoms until the disease is advanced. Signs and symptoms of pancreatic cancer are as follows-
- Loss of weight
- Loss of appetite
- Itching
- Diabetes
- Swelling and pain in arms or legs
- The pain could be due to a blood clot
- Weakness
- Tiredness
- Jaundice
Causes
There is no particular cause that has been found for pancreatic cancer. Medical professionals and doctors have found some reasons that may raise the risk of this cancer. These reasons include- having a family history of pancreatic cancer or smoking.
Risk factors
Factors that may raise the risk of pancreatic cancer are as follows –
- Type 2 diabetes
- Smoking
- Pancreatitis (which is also known as chronic inflammation of the pancreas)
- A family history of DNA changes increases cancer risk. These include changes in the BRCA2 gene, familial atypical multiple mole melanoma (FAMMM) Syndrome, and Lynch syndrome.
- Family history of pancreatic cancer
- Obesity
Complications
As pancreatic cancer grows and spreads it causes complications like
Loss of weight – Various people with pancreatic cancer lose weight as this type of cancer uses more of the body’s energy.
Vomiting and nausea caused by treatment of this cancer or cancer pressing on the belly might make it difficult to eat.
This type of cancer blocks the liver’s bile duct which can cause jaundice. Yellowing of skin and the whites of the eyes are some of the signs. Jaundice can cause pale stools and dark-colored urine. It usually occurs without stomach pain.
If the bile duct is blocked, a metal or plastic tube called a stent is put inside. This stent helps to hold the bile duct open. All this is done using a procedure called endoscopic retrograde cholangiopancreatography which is also called ERCP.
During ERCP, a gastroenterologist puts a long tube with a small camera called an endoscope down the throat. This tube goes down through the stomach and into the upper part of the intestine (small intestine). The doctor also put a dye into the pancreatic ducts and bile ducts through a tiny tube that fits through the endoscope. The dye helps to show up the ducts on imaging tests.
Pain- an aggressively growing tumor might press on nerves present in your abdomen. Causing a severe pain. Treatments such as chemotherapy and radiation might help to slow the tumor’s growth and help reduce the pain.
If medicines aren’t helping. Doctors suggest a celiac plexus block. This procedure uses a needle to put alcohol in the nerves that control pain in the stomach. The alcohol infused in the nerves stops the nerves from sending pain signals to the brain.
Bowel blockage – pancreatic cancer can grow on the first part of the small intestine known as the duodenum. Which can block the flow of digested food from the stomach into the intestines.
When to see a surgical gastroenterologist who specializes in pancreatic cancer surgery?
Visit a surgical gastroenterologist if you have the symptoms that are bothering you.
Pancreatic Cancer Treatment in Hyderabad
The best and the only reliable option to cure pancreatic cancer is surgery.
It is possible to remove or resect all cancer when test results indicate potentially curative surgery. But, if the cancer has widespread, then palliative surgery is done to prevent complications and to get rid of symptoms.
Only 20% of pancreatic cancers remain confined to the pancreas when they are first diagnosed. In most cases, complete resection becomes difficult when the cancer spreads too far away.
Surgical Treatment for Pancreatic Cancer
Whipple procedure (pancreaticoduodenectomy)
The most common and reliable procedure to remove pancreatic cancer is pancreaticoduodenectomy (Whipple procedure). In this procedure, an expert surgeon removes the head part of the pancreas or the body of the pancreas. Sometimes, a part of the small intestine, bile duct, lymph nodes, and gallbladder are removed.
Learn more about the “Whipple Procedure”
It can be done in both ways: open as well as laparoscopically.
Distal pancreatectomy
Pancreatic cancer confined to the body and tail of the pancreas is removed by a distal pancreatectomy procedure. Speen is also removed (splenectomy) during this procedure.
Total pancreatectomy
This operation removes the entire pancreas, the gallbladder and common bile duct, part of the stomach and small intestine, and the spleen.
Prevention
Screening is done for people with a greater risk of pancreatic cancer. Screening uses tests to look for signs of pancreatic cancer that do not show any symptoms. Screening involves imaging tests such as ultrasound and MRI.
The main objective of screening is to find whether the pancreatic cancer is small or can be cured.
Another type of testing known as genetic testing is done to find DNA changes that run in families and increase the risk of pancreatic cancer.
Ways to lower the risk of pancreatic cancer
Stop smoking- If you smoke, then talk to a specialist about the ways and therapies to stop smoking. Some of the potential therapies might include nicotine replacement therapy and medicines.
Maintain a healthy weight. Exercise regularly. Choose a vegetable-rich diet with fruits and whole grains in smaller amounts.
Stop consuming alcohol
If you are looking for the best pancreatic cancer treatment in Hyderabad, then meet Dr. Datta Ram U.