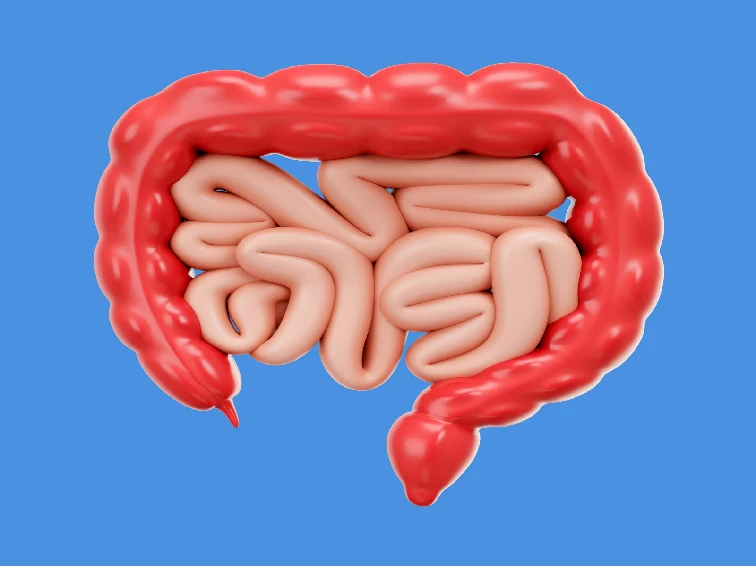
Intestinal pseudo-obstruction is a medical condition characterized by a disruption in the normal movement of the intestines. It can lead to symptoms similar to those of a mechanical bowel obstruction, such as abdominal pain, bloating, and constipation. However, in intestinal pseudo-obstruction, there is no physical blockage in the intestines. In this article, we will delve into the details of this condition, including its causes, symptoms, and available treatment options.
1. Introduction
Intestinal pseudo-obstruction refers to a condition where there is a functional impairment in the movement of the intestines, mimicking the symptoms of a mechanical bowel obstruction. It can affect both the small and large intestines and can be a chronic or acute condition.
2. Understanding Intestinal Pseudo-Obstruction
2.1 Intestinal Pseudo-Obstruction Causes
Intestinal pseudo-obstruction can be categorized into two types: primary and secondary. Primary intestinal pseudo-obstruction, also known as chronic idiopathic intestinal pseudo-obstruction, has no identifiable cause. Secondary intestinal pseudo-obstruction, on the other hand, occurs due to an underlying medical condition or as a result of certain medications.
Several factors can contribute to the development of secondary intestinal pseudo-obstruction, including:
• Neurological disorders
• Connective tissue diseases
• Serious Infections
• Trauma
• Cardiac disease (Heart attack and congestive heart failure)
• Medications (e.g., opioids, anticholinergics)
• Metabolic disorders
• Autoimmune conditions
2.2 Intestinal Pseudo-Obstruction Symptoms
Intestinal pseudo-obstruction causes a variety of symptoms based on the location and severity of the condition. Common symptoms include:
• Abdominal pain and cramping
• Bloating and abdominal distention
• Nausea and vomiting
• Constipation or diarrhea
• Loss of appetite
• Weight loss
• Severe abdominal pain
• Feeling incomplete evacuation after bowel movements
• Feeling like gas that you cannot pass
• Cramps
3. Diagnosis and Medical Evaluation
To diagnose intestinal pseudo-obstruction, a comprehensive medical evaluation is necessary. The following steps may be involved in the diagnostic process:
3.1 Medical History and Physical Examination
Your gastroenterologist will review your medical history and perform a physical examination to assess your symptoms and identify any underlying conditions that may contribute to intestinal pseudo-obstruction.
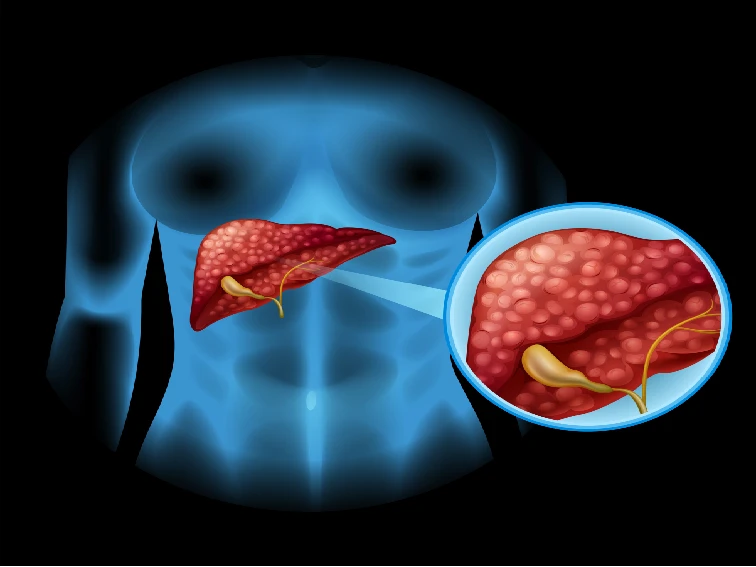
3.2 Imaging Tests
Imaging tests such as X-rays, CT scans, and MRI scans may be conducted to visualize the intestines and identify any abnormalities or signs of obstruction. These imaging tests provides complete details that are not visible through other imaging tests.
3.3 Gastric Emptying Study
A gastric emptying study involves consuming a meal containing a small amount of radioactive (nuclear) material. The movement of the meal through the stomach and intestines is tracked to evaluate the motility of the digestive system.
Gastroduodenal manometry: A gastroenterologist passes a small flexible tube with a small camera and instruments through the esophagus. The doctor performs this procedure to see how often the smooth muscles in the stomach and small intestine contracts and relaxes.
4. Treatment Options for Intestinal Pseudo-Obstruction
The treatment approach for intestinal pseudo-obstruction aims to alleviate symptoms, improve intestinal motility, and manage any underlying causes. The following treatment options may be considered:
4.1 Medications
Medications such as prokinetic agents, which enhance intestinal contractions, may be prescribed to improve the movement of the intestines. Additionally, pain medications and antiemetics may be used to manage symptoms.
4.2 Nutritional Support
In cases where malnutrition or dehydration occurs, nutritional support may be necessary. This can involve intravenous fluids, tube feeding, or dietary modifications to ensure adequate nutrient intake.
4.3 Surgical Intervention
Surgery may be required in certain cases of intestinal pseudo-obstruction. It can involve removing any obstructions, repairing damaged areas, or bypassing sections of the intestines to restore normal bowel function.
5. Managing Intestinal Pseudo-Obstruction: Lifestyle and Home Remedies
While medical interventions are crucial, managing intestinal pseudo-obstruction also involves certain lifestyle modifications and home remedies. These may include:
• Eating smaller, more frequent meals
• Chewing food thoroughly
• Staying well-hydrated
• Engaging in regular physical activity, as tolerated
• Reducing stress levels through relaxation techniques
6. Prevention and Outlook
As primary intestinal pseudo-obstruction has no known cause, specific preventive measures are not available. However, managing underlying conditions and following the prescribed treatment plan can help alleviate symptoms and improve quality of life.
The outlook for individuals with intestinal pseudo-obstruction varies depending on the underlying cause and the effectiveness of treatment. With proper medical management and lifestyle modifications, many people can lead fulfilling lives despite the challenges posed by this condition.
7. Conclusion
Intestinal pseudo-obstruction is a complex medical condition that affects the normal movement of the intestines. It can lead to distressing symptoms such as abdominal pain, bloating, and constipation. Early diagnosis and appropriate treatment are essential for managing the condition and improving the quality of life for affected individuals. If you suspect you may have intestinal pseudo-obstruction or are experiencing persistent gastrointestinal symptoms, consult a healthcare professional for a thorough evaluation and guidance.
8. FAQs
Q1: Is intestinal pseudo-obstruction a rare condition?
Intestinal pseudo-obstruction is considered a rare condition, but its exact prevalence is not well established.
Q2: Can intestinal pseudo-obstruction be cured?
While there is no cure for intestinal pseudo-obstruction, symptoms can often be managed through a combination of medical interventions and lifestyle modifications.
Q3: Can stress worsen the symptoms of intestinal pseudo-obstruction?
Stress can potentially exacerbate the symptoms of intestinal pseudo-obstruction. Managing stress through relaxation techniques and stress-reducing activities may be beneficial.
Q4: Can intestinal pseudo-obstruction affect people of all ages?
Yes, intestinal pseudo-obstruction can affect individuals of all ages, including children and adults.
Q5: Are there any support groups or organizations for individuals with intestinal pseudo-obstruction?
Yes, there are support groups and organizations dedicated to providing resources and support to individuals living with intestinal pseudo-obstruction.