Hernia Treatment in Hyderabad | Dr. Datta Ram U
A hernia is a condition that is common but not fully understood by many. If you have swelling and a protrusion that can be pushed back into your abdomen, you may be experiencing a hernia. If it continues to increase in size, surgery may be necessary to repair it. We will examine the causes of hernias, the various types of hernias, and how our state-of-the-art robotic surgery can assist individuals requiring hernia repair.
If you have hernia…
The most prevalent indication is the bulge that sticks out, revealing that an organ or intestine is pushing through the muscular wall. This enlargement may cause discomfort and increase in size. When lifting, certain individuals may also feel a persistent soreness.
When do you need surgery for hernia?
In certain situations, if the hernia is insignificant, remains stable in size, and doesn’t cause any discomfort or complications, then there might not be an immediate need for surgery.
Hernia can cause problems
Nonetheless, it’s crucial to understand that in most cases, hernias tend to increase in size over time. Even if it isn’t problematic presently, there is a high possibility that it could lead to severe complications later on if it’s not treated.
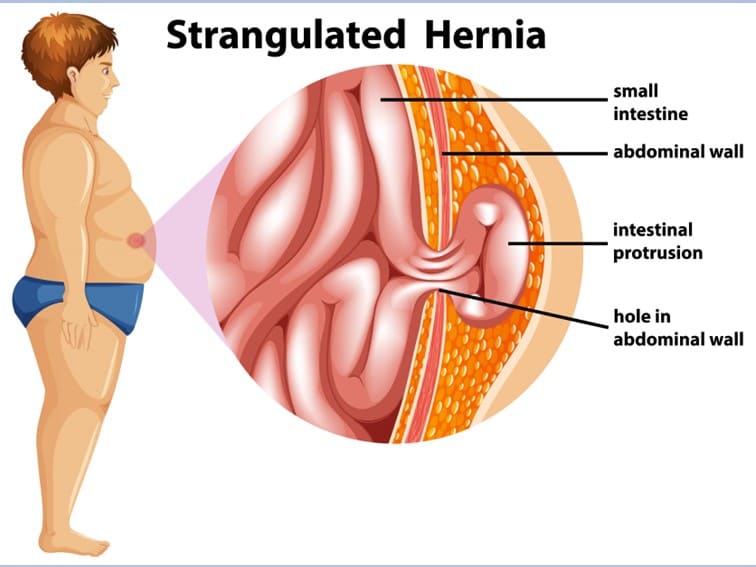
Strangulation
One of the possible complications is strangulation, which takes place when the protruding tissue gets compressed by the muscle wall, resulting in the blockage of blood supply and subsequent tissue death.
Hernia Complications
If a hernia becomes strangulated, it can lead to long-term harm and require immediate surgical intervention. Typically, the affected organs, such as the intestines, will become necrotic and could result in severe illness if not promptly removed. Therefore, it’s crucial to contact your surgical gastroenterologist right away if you experience symptoms like fever, nausea, sudden worsening pain, or if your hernia changes color to red, purple, or dark.
If Your Hernia Causes problems…
You will experience fever, intense pain, nausea, vomiting, the bulge that turs purple or red, progressive pain and discomfort.
Hernia Treatment in Hyderabad
Experienced surgical gastroenterologists recommend surgery to prevent potential complications. Doctors advise patients to undergo a minimally invasive laparoscopic hernia repair procedure to treat hernia. The procedure helps in preventing hernia from getting worse or doesn’t allow it to increase in size.
Laparoscopic hernia repair surgery
Recent developments in minimally invasive surgery allow for procedures to be carried out using only a few small incisions instead of a larger “open” incision, providing patients with a less invasive option. Laparoscopic surgery is also utilized for other procedures like gallbladder removal and weight loss surgery.
Bottom Line
It is crucial that you make an appointment for your surgery without delay, as postponing it may lead to more severe complications in the future. If you suspect that you have a hernia or require additional information, please get in touch with Dr. Datta Ram right away, and he will provide you the best hernia treatment in Hyderabad.