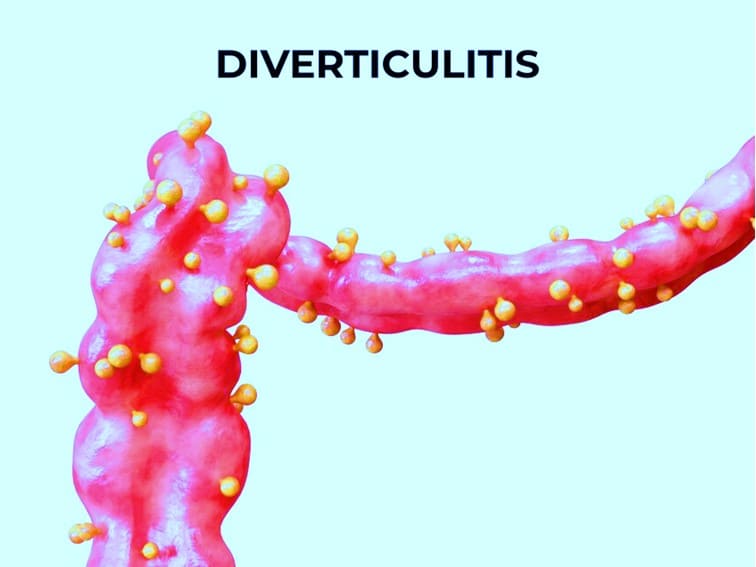
Older people may develop small bulges or pockets (diverticula) in their intestinal lining. In a majority of people, diverticula do not cause any symptoms. In such cases, people get to know about their condition only when they get scanning done for another reason. When there are no symptoms, the condition is known as diverticulosis. However, when diverticula cause symptoms such as abdominal pain. The condition is known as diverticular disease. When diverticula become infected or inflamed more severe symptoms may manifest. The condition is known as diverticulitis.
Symptoms of Diverticular disease and diverticulitis
Abdominal pain is usually in the left side of the abdomen. The pain looks intermittent. It comes and goes – but may get severe after eating. Farting and bowel movements ease the pain. The other symptoms may include diarrhea, constipation, or both. Infection and inflammation of diverticula (diverticulitis) is associated with more severe abdominal pain, constipation, and severe diarrhea. The other symptoms may include mucus and blood in the stools and rectal bleeding. These symptoms may also be due to other serious health conditions – such as colorectal cancer. Therefore, one must not ignore such symptoms.
Furthermore, having one or more of these symptoms doesn’t always mean that you have diverticulitis. Other gastrointestinal disorders such as stomach ulcers, gallstones, appendicitis, inflammatory bowel disease, celiac disease, and irritable bowel syndrome can also cause similar symptoms.
Who are at risk of developing diverticulosis and diverticulitis?
The risk of developing the diverticular disease is high if you:
- Are obese
- Are Male
- Are above age 40 years
- Eat red meat and diet high in fat
- Eat a diet lacking fiber
- Don’t eat legumes, beans, vegetables, and fruits
- Don’t exercise
- Take NSAIDs
- Smoke
How is diverticulitis diagnosed?
You must see a gastroenterologist if you develop any of the above-mentioned symptoms. Your doctor will also ask you about your symptoms, lifestyle, dietary habits, medical history, bowel habits, and any medicines that you are taking. The doctor may order a few tests after a thorough physical examination. The tests may include blood tests, stool culture, rectal examination, a CT scan, and sigmoidoscopy or colonoscopy. These tests are helpful in the diagnosis of diverticulitis.
Bottom Line
You’re more likely to get diverticular disease and diverticulitis if you do not get enough fiber in your diet. If your diverticulitis is due to an infection or other cause, your gastroenterologist will treat the condition with antibiotics. Mild diverticulitis can be prevented by drinking lots of water, exercising, and taking a high-fiber diet. For severe and chronic cases of diverticulitis, surgery may be required.