Best doctor for IBD in Hyderabad Dr. Datta Ram U explains IBS in simple terms for a layman to understand it better for better management.
What is IBS Inflammatory Bowel Disease?
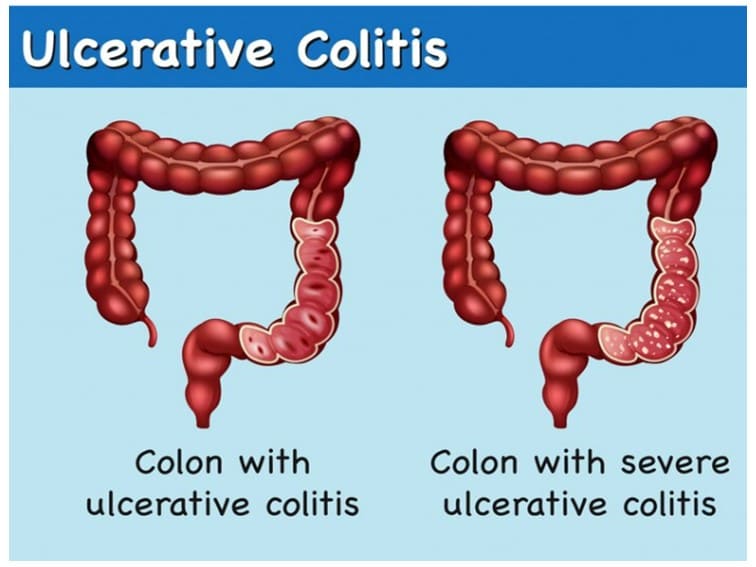
Irritable bowel disease is an inflammatory condition of the large intestine. People who have this condition suffer from abdominal pain, cramping, constipation, diarrhea, bloating, and gas. It is a chronic condition that needs to be managed on a long-term basis.
Though this is a common health issue only a few people with IBD have severe signs and symptoms. The best way to manage this condition is by managing stress, anxiety, lifestyle, and diet. For more severe and nagging symptoms diet, medications, lifestyle, and counseling can help.
IBS doesn’t cause changes in bowel tissue or increase your risk of colorectal cancer.
What are the signs and Symptoms of IBD?
IBD Symptoms – symptoms may vary but may last longer. Common symptoms may include bloating, indigestion, cramping, inflammation, abdominal pain, passing mucus in stools, changes in bowel habits, changes in the frequency of bowel movements, and increased gas or mucus in stools.
Is there any precise cause of IBS?
IBS Causes – So far there is no known or specific cause associated with this condition. The following factors could play a role:
Early childhood stress: This may be the reason for IBS in some people. Those who were exposed to stressful events during their early childhood days tend to have IBD-associated symptoms during their adulthood and continue to have them for a long time.
Gastrointestinal infection: In some people, IBS can develop after severe diarrhea or gastroenteritis caused by a virus or bacterial disease. Bacterial overgrowth can also cause IBS symptoms. Disturbance in the balance of normal gut bacteria (microbial flora) of the gut can also cause IBS symptoms.
Nervous system abnormalities can cause discomfort in the abdominal muscles due to improper and poorly coordinated signals from the brain and intestines. This may result in pain, constipation, and diarrhea.
Stronger and longer intestinal muscle contractions can cause bloating, gas and diarrhea.
What triggers IBS?
Some people experience worse IBS symptoms when they eat or drink certain foods or beverages, carbonated drinks, milk, cabbage, beans, citrus fruits, dairy products, and wheat.
Stress: In some people, stress may trigger IBS symptoms or can make IBS symptoms worse, but doesn’t cause them.
What are the risk factors for IBS?
A strong family history – genes and environmental factors could play a role.
A history of stress, anxiety, depression, and emotional and sexual abuse can make the condition worse.
Sex – females are more prone to it compared to males and the condition is common in young females.
What are the complications associated with IBS?
Chronic diarrhea and constipation can cause Hemorrhoids. Those who have chronic IBS and associated moderate to severe symptoms regularly may have a poor quality of life. They also miss work more often compared to others. People with IBS are more prone to stress, anxiety, and depression and also people with stress and depression may have worse IBS symptoms.
When should you see a specialist doctor?
If you are searching for the best doctor for IBD in Hyderabad, you should not worry much unless you have the following signs and symptoms:
- Persistent diarrheas – especially at night
- Iron deficiency
- Frequent abdominal cramps
- Persistent abdominal pain
- Nauseas & vomiting sensation
- Rectal bleeding and other uncommon symptoms.